Table of Contents
Hapten
Haptens are small-molecular-weight compounds that evoke an immune response only when they are attached to carrier proteins. In vivo, haptens readily bind to serum proteins such as albumin. The combined molecular weights of albumin and the hapten need to exceed 3000 MW to stimulate the immune system. The immune response is directed at both the hapten and the carrier protein. The carrier protein has a different and antigenic structure after binding to the hapten. The concept of haptens was introduced by Landsteiner. Subsequently, experiments with murine models demonstrated that immunization with m-aminobenzene sulfonate failed to elicit an immune response (Figure 3-3).
However, a vigorous antibody response was observed when m-aminobenzene sulfonate was linked to carrier protein (ovalbumin).
Antibodies were directed to both the aminobenzene and the carrier protein. The phenomenon was termed haptenic response, from the Greek haptein, which means “to fasten.”
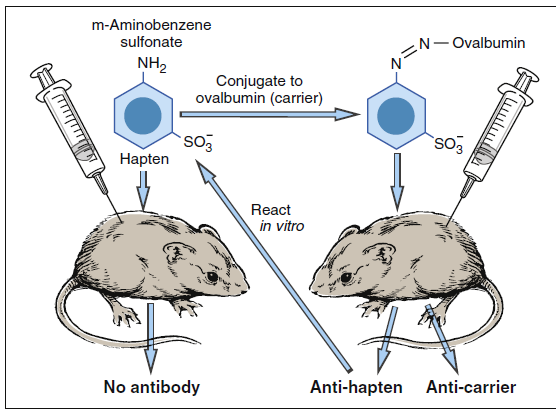
Hapten conjugation to ovalbumin.
Pharmaceuticals as Haptens
Most pharmaceuticals and antibiotics are small (at or less than 3000 MW) compounds. The native drug or metabolites are often haptens that bind to serum proteins or molecules expressed on cells and elicit either an antibody response or a cellular response. An immune response to the hapten carrier complex can result in skin eruptions, asthma, anaphylaxis, and autoimmune reactions. Antibiotics and anesthetics are common biologically active haptens.
Antibiotics as Haptens
Penicillin is the leading cause of immunologically mediated adverse health effects. Approximately 2% of patients receiving penicillin therapy develop urticaria, asthma, or angioedema.
Anaphylaxis, which is a serious and often fatal reaction to penicillin, results in 500 to 1000 deaths each year in the United States. Penicillin is composed of an acyl side chain linked to a β-lactam ring combined with a thiazolidine ring. Natural penicillin (PenG), penicillinase-resistant penicillins (methicillin), extended-spectrum penicillin (amoxicillin), and broad-spectrum penicillin (carbenicillin) all have the same core β-lactam ring, which is essential for antimicrobial activity. Bacteria secrete a β-lactamase that breaks the lactam ring, rendering the
antibiotic ineffective and creating highly charged metabolites (Figure 3-4). The major antigenic determinant (90%–95% of the breakdown products) is a benzylpenicilloyl derivative (BPO). Minor metabolites include parental penicillin, penicilloate, and penicilloylamine. Major and minor metabolites combine with proteins to become immunogenic.
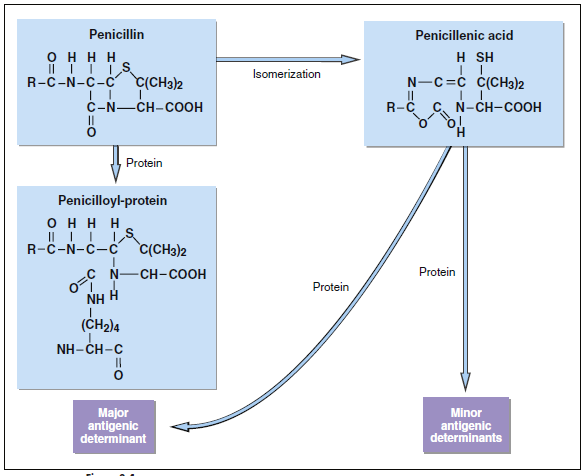
Penicillin haptenic metabolites. The conjugation of penicilloyl derivatives to protein via an amide linkage
is shown in the lower left.
Cephalosporins have a structure that is similar to penicillin and is reactive haptens. For reasons that are unclear, third (ceftriaxone) and fourth (cefepime) generations of cephalosporins are more involved in immunologically mediated adverse health effects. The haptenic determinants of cephalosporin are not fully delineated. It has been suggested that serologic reactivity is directed at both the acyl side chains and the β-lactam ring linked to the carriers.
Anesthetics as Haptens
Exposure to halothane may also induce an autoimmune reaction. Introduced in 1951 as a potent, nonflammable anesthetic agent, halothane is metabolized in oxidative pathways to trifluoroacetyl chloride (TFAC). In a subsequent chemical reaction, TFAC acetylates liver proteins to form a neoantigen. An immune response to the neoantigen causes halothane hepatitis. Inflammation of the liver abates when the drug is discontinued.
Pharmaceuticals and Neoantigens
Highly reactive haptens readily bind to red blood cell membranes to create immunogenic neoantigens (Box 3-1). For example, methyldopa binds to the red blood cell membrane, thus creating a neoantigen. A hemolytic anemia results when antibodies react with the neoantigen and lyse the red cells.
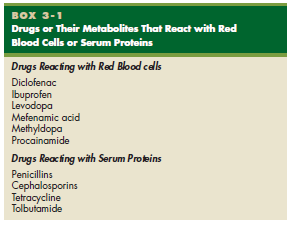
Blood Cells or Serum Proteins
Haptens and Cell-Mediated Reactions
Some responses to pharmaceuticals are mediated by inflammatory cells rather than by antibodies. Skin lesions, which are characterized by redness, induration, or blistering, occur 24 to 48 hours after exposure and are mediated by CD4Th1 cells and inflammatory macrophages. Inflammatory responses in the liver and kidney have also been reported. Clinical symptoms may persist after discontinuation of the drug. Delayed hypersensitivity reactions in the skin or cutaneous drug reactions (CDRs) occur following systemic
administration of a wide variety of drugs. Antimicrobial agents (sulfonamides), anticonvulsants (carbamazepine), anesthetics (lidocaine), anti-psychotics (clozapine), cardiovascular agents (procainamide, hydrazaline) and nonsteroidal anti-inflammatory drugs (diclofenac) are metabolized by the liver with the creation of reactive haptens, which bind to skin cells. An inflammatory response in the skin is characterized by widespread rashes and eruptions. Reactions in the skin usually occur 7 to 10 days after drug administration.