TCR (T Cell Receptor) or co-stimulatory molecule interactions with APC receptors are disrupted or prevented by biotechnology-derived immunotherapeutic drugs. In this diagram, monoclonal antibodies and fusion proteins that stop T cells from activating are displayed given below figure.
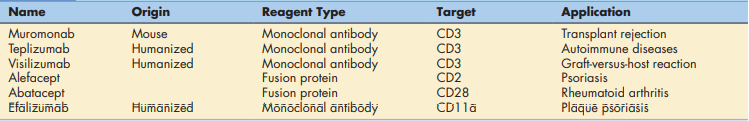
Table of Contents
Blockade of T Cell Receptor Interactions
Monoclonal antibodies made in the lab (muromomab, teplizumab, and visilizumab) bind to CD3 on activated T cells. Blocking antibodies inhibit CD3 from interacting with class I or II molecules, which can lead to recipient graft rejection and, in rare circumstances, the graft rejecting the host.
Blockade of Co-Stimulatory Molecule Interactions
Biotechnology-derived fusion proteins or monoclonal antibodies can inhibit the interaction between co-stimulatory factors on T cells and APCs. Two genes are fused in the lab and put into an expression vector, such as a bacterium or yeast, to make a fusion protein. The active parts of both proteins are combined in the fusion protein when it is translated. Currently, two fusion proteins are utilized to prevent T cells and APCs from interacting with co-stimulator molecules.
Abatacept is a co-stimulator inhibitor in a new class of drugs called disease-modifying antirheumatic drugs (DMARDs). In patients with rheumatoid arthritis, T cell activation is the major cause of the inflammatory response in the synovium. Abatacept consists of an Fc region from the immunoglobulin G (IgG) antibody and the extracellular domain of CTLA-4. The CTLA-4 fusion protein physically blocks the interaction between CD28 and the B7 on APCs. Failure to engage CD28 drives activated T cells into apoptosis.
Alefacept is another fusion protein indicated for psoriasis Vulgaris, an autoimmune skin disease. Activated CD4, CD8, and memory cells are found in skin lesions. Alefacept prevents T cell activation and reduces the severity of the lesions. The fusion protein consists of LFA-3 (CD58) linked to the distal end of an antibody molecule. Interactions between the soluble alefacept and the T cell CD2 molecule block the binding of CD2 to the CD58 on APCs.
Monoclonal antibodies, which inhibit co-stimulatory molecules, are also indicated for the treatment of psoriasis. For example, efalizumab blocks interactions between the CD11a component of LFA-1 and the adhesion factors on APCs. Again, downregulation of T cells reduces the severity of skin lesions.
Aberrant interactions between tcr and class ii molecules
Superantigens
Superantigens are molecules that activate up to 20% of all T lymphocytes (typical antigen response stimulates just 0.01 percent of T cells), causing them to produce large amounts of proinflammatory cytokines like tumour factor– (TNF-). TNF- causes life-threatening hypovolemic shock and organ failure when released into the bloodstream.
Superantigens work in a unique way to activate CD4 cells. The bridging of the constant area of class II molecules and the variable portions of the TCR-chain (V) brings T cells and APCs into close contact. Superantigen binding, on the other hand, is distinct in because it takes place outside of the usual binding clef showing in below figure.
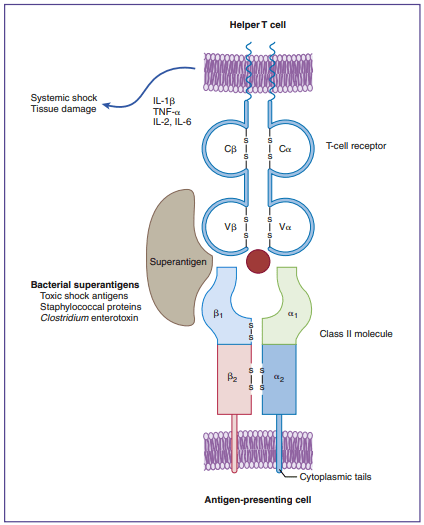
Staphylococcal and streptococcal superantigens have been implicated in food poisoning, exfoliative dermatitis in infants (scalded skin syndrome), cellulitis, scarlet fever, and toxic shock syndrome. Staphylococcus aureus secretes five entero[1]toxins (SEA, SEB, SEC2, SEE, and TSST-1). Enterotoxins are similar to exotoxins but usually only cause moderate to severe diarrhea. All staphylococcal enterotoxins can cause the symp[1]toms of food poisoning, but only SEA and SEB are involved in exfoliative dermatitis. Toxic shock syndrome is associated with the TSST-1, SEB, or SEC2 superantigens. In the last 20 years, an increase has been seen in the inci[1]dence of streptococcal toxic shock syndrome associated with necrotizing fasciitis or myositis. The etiologic agents are invasive Group A streptococcal strains such as Streptococcus pyogenes. These strains produce three different superantigens (SPE-A, SPE-B, and SPE-C) and numerous pyogenic toxins. SPE-A is specifically associated with streptococcal toxic shock syndrome (sTSS). Streptococcal and staphylococcal superan[1]tigens act in a similar manner.
Make sure check our amazing article related to this post: Surface Interactions Between T Cells and Antigen-Presenting Cells