Injury to tissue may result in cell death and tissue destruction. Healing, on the other hand, is the body’s response to injury in an attempt to restore normal structure and function.
The process of healing involves two distinct processes:
Regeneration: When healing takes place by the proliferation of parenchymal cells and usually results in complete restoration of the original tissues.
Repair: When the healing takes place by the proliferation of connective tissue elements results in fibrosis and scarring.
Table of Contents
Process of healing
1. Regeneration
Some parenchymal cells are short-lived while others have a long life span. In order to maintain proper structure of tissue, these cells are under the constant regulatory control of their cell cycle. These include growth factors such as epidermal growth factor, fibroblast growth factor; platelet-derived growth factor, and endothelial growth factor.
Regeneration of any type of parenchymal cells involves the following two processes.
• Proliferation of original cells form the margin of injury with migration so as to cover the gap.
• Proliferation of migrated cells with subsequent differentiation and maturation so as to reconstitute the original tissue. Depending upon their capacity to divide, cells of the body can be divided into three groups.
I. Labile cells: These cells continue to multiply throughout life under normal physiologic conditions. These include surface epithelial cells of the epidermis, alimentary tract, respiratory tract, urinary tract, vagina, cervix, uterine endometrium, haemotopoietic cells of bone marrow, and cells of lymph nodes and spleen.
II. Stable cells: These cells decrease or lose their ability to proliferate after adolescence but retain the capacity to multiply in response to stimuli throughout adult life. These include parenchymal cells of organs like the liver, pancreas, kidneys, adrenal, and thyroid. Mesenchymal cells like smooth muscle cells, fibroblasts vascular endothelium bone, and cartilage cells.
III. Permanent cells: These cells lose their ability to proliferate around the time of birth. These include neurons, skeletal muscle, and cardiac cells.
2. Repair
Repair is the replacement of injured tissue by fibrous tissue. These responses take place by the participation of mesenchymal cells (consisting of connective tissue, stem cells fibrocytes, and histocytes).
The process of repair involves I. Granulation tissue formation II. Contraction of wounds.
I. Granulation Tissue Formation:
The term granulation tissue derives its name from the slightly granular and pink appearance of the tissue. Each granule corresponds histologically to the proliferation of new small blood vessels which are slightly lifted on the surface by the covering of fibroblasts and young collagen. The following three phases are observed in the formation of granulation tissue.
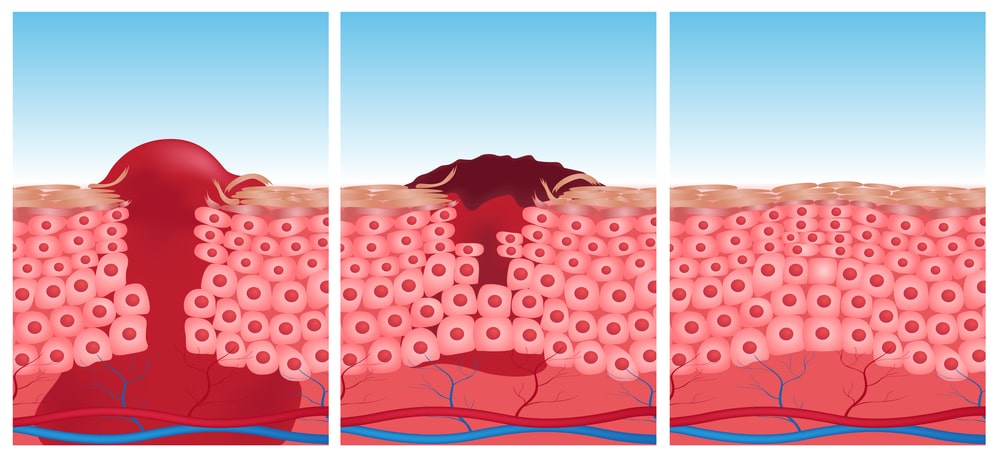
- Phase of inflammation: Following trauma, blood clots at the site of injury. There is an acute inflammatory response with exudation of plasma, neutrophils, and some monocytes within 24 hours.
- Phase of clearance: Combination of proteolytic enzyme liberated from neutrophils autolytic enzymes from dead tissue cells and phagocytic activity of macrophages clear off the necrotic tissue, debris, and red blood cells.
- Phase of growths of granulation tissue: This phase consists of two main processes.
(i) Angiogenesis Formation of new blood vessels at the site of injury takes place by the proliferation of endothelial cells from the margins of several blood vessels. Initially, the proliferated endothelial cells are solid buds but within a few hours develop into the lumen and start carrying blood. The newly formed blood vessels are leakier, accounting for the edematous appearance of new granulation tissue. Soon these blood vessels differentiate into muscular arterioles, thin-walled venules, and true capillaries.
(ii) Fibrogenesis The newly formed blood vessels are present in an amorphous ground of surface matrix. The new fibroblasts originate from fibrocytes as well as the mitotic division of fibroblasts. Some of these fibroblasts have a combination of morphologic and functional characteristics of smooth muscle cells. Collagen fibrils begin to appear by about 6 th day. As maturation proceeds, more and more collagen is formed while the number of active fibroblasts and new blood vessels decreases. This results in the formation of inactive-looking scars.
II. Contraction of Wounds:
The wound starts contracting after 2-3 days and the process is completed by the 14th day. During this period the wound is reduced by approximately 80% of its original size. A contracted wound results in rapid healing since the lesser surface area of the injured tissue has to be replaced. In order to explain the mechanism of wound contraction a number of factors have been proposed.
- Dehydration as a result of removal of fluid by drying of wound was first suggested but without being substantiated.
- Contraction of collagen was thought to responsible for contraction but wound contraction proceeds at a stage when the collagen content of granulation tissue is very small.
- Discovery of myofibroblasts appearing in active granulation tissue has resolved the controversy. These cells have features intermediate between those of fibroblasts and smooth muscle cells. Their migration into the wound area and their active contraction decreases the size of defect.
Also Read: What are Inflammatory Mediators