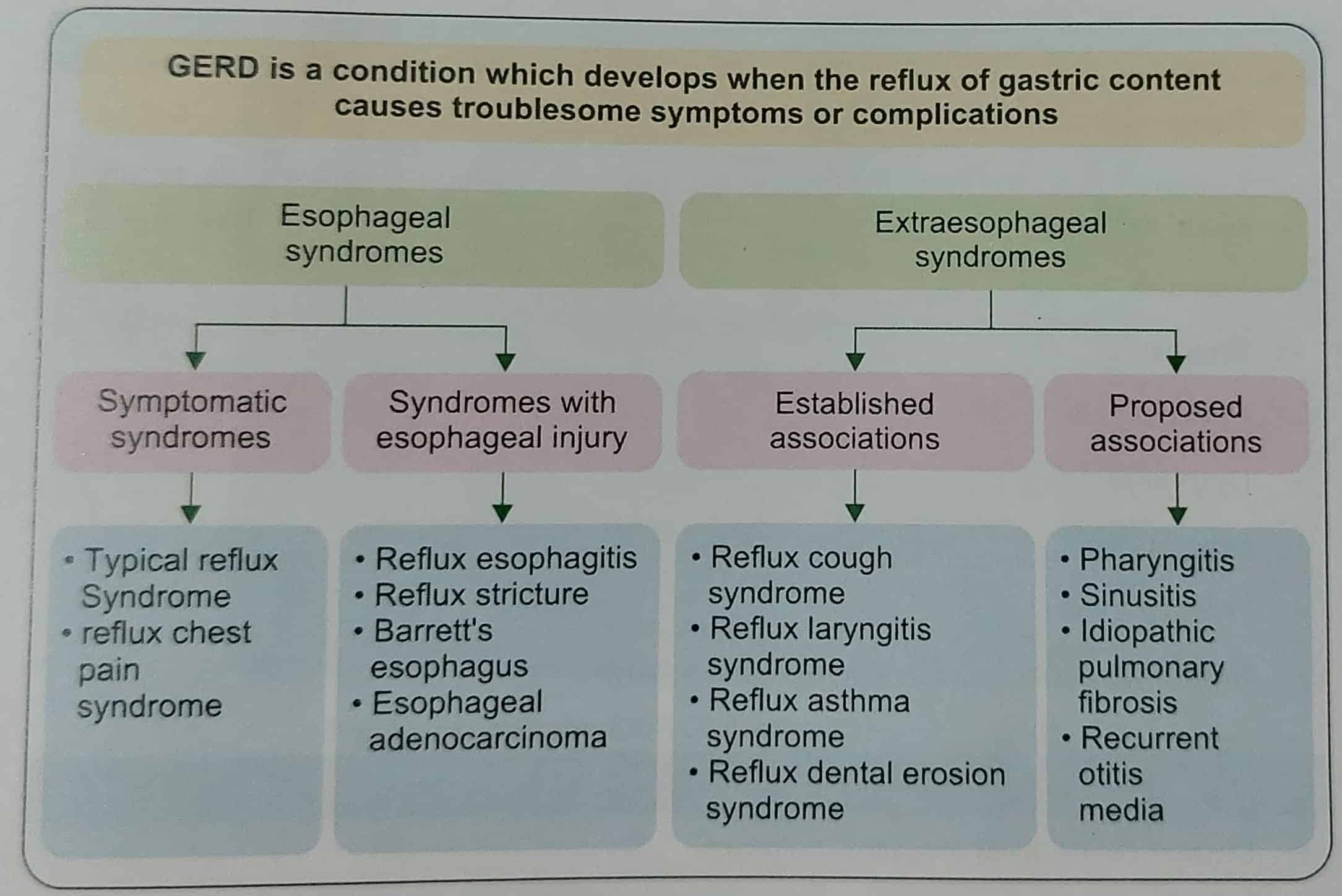
Gastroesophageal reflux disease (GERD) is a condition that develops when the reflux of stomach contents into the esophagus causes troublesome symptoms and/or complications. According to the Montreal definition of GERD, GERD can be classified into esophageal and extraesophageal syndromes (Fig. 1). Patients with GERD can present with typical or atypical symptoms. If there is evidence of syndromes with an esophageal injury like reflux esophagitis, reflux stricture, Barrett’s esophagus, or esophageal adenocarcinoma, a diagnosis of GERD is confirmed and no further diagnostic testing is required.
Table of Contents
TRIAL OF ACID SUPPRESSIVE MEDICATIONS
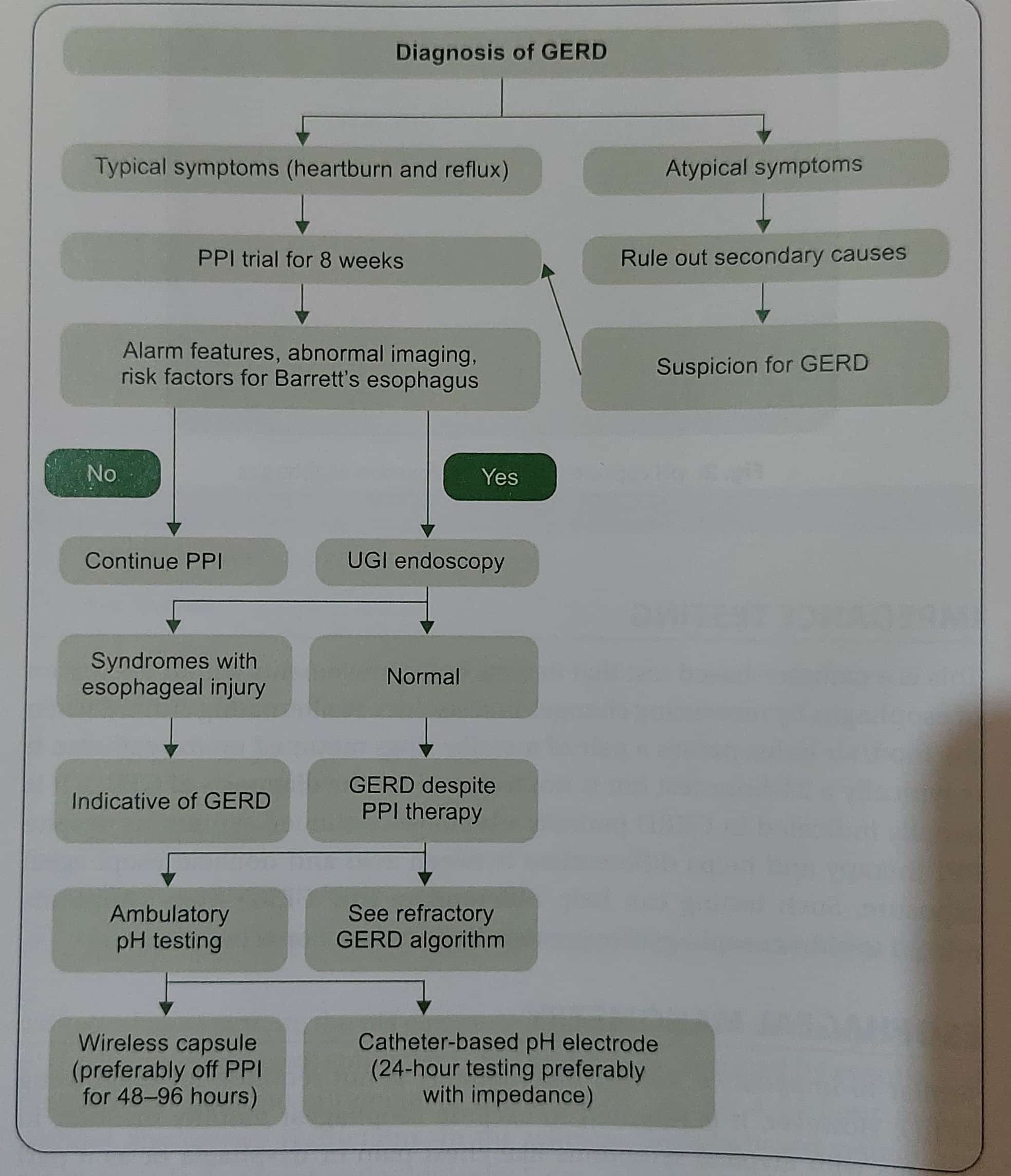
A diagnosis of GERD in patients with typical symptoms (such as heartburn and/or acid regurgitation) can be made by a trial of PPI therapy. Usually, the trial consists of once-daily proton pump inhibitor (PPI) therapy, given before breakfast, for a duration of 8 weeks.2 A multicenter, prospective, randomized controlled study indicated that the incidence of symptom relapse was higher for the 4-week group than 8-week group (62.5% vs. 47.8%; difference, 14.7%; 95%confidence interval, 3.7-25.7%; P = .009).
For patients with atypical symptoms (such as chronic cough, hoarseness of voice), other causes need to be ruled out that could be mimicking GERD, for example, an extensive cardiac workup would be required if the patient presents with chest pain. Pulmonary causes would need to be ruled out for patients with cough or shortness of breath.
UPPER GI ENDOSCOPY
In patients with refractory GERD (who do not respond to PPI trial), or those with alarm features (Box 1), abnormal upper GI imaging like a barium esophagram or risk factors for Barrett’s esophagus (Box 2), an upper GI endoscopy would be indicated. If there is evidence of syndromes with esophageal injury (as listed above; for example erosive esophagitis), that itself would indicate GERD.
Products to manage your acidity
AMBULATORY ESOPHAGEAL pH TESTING
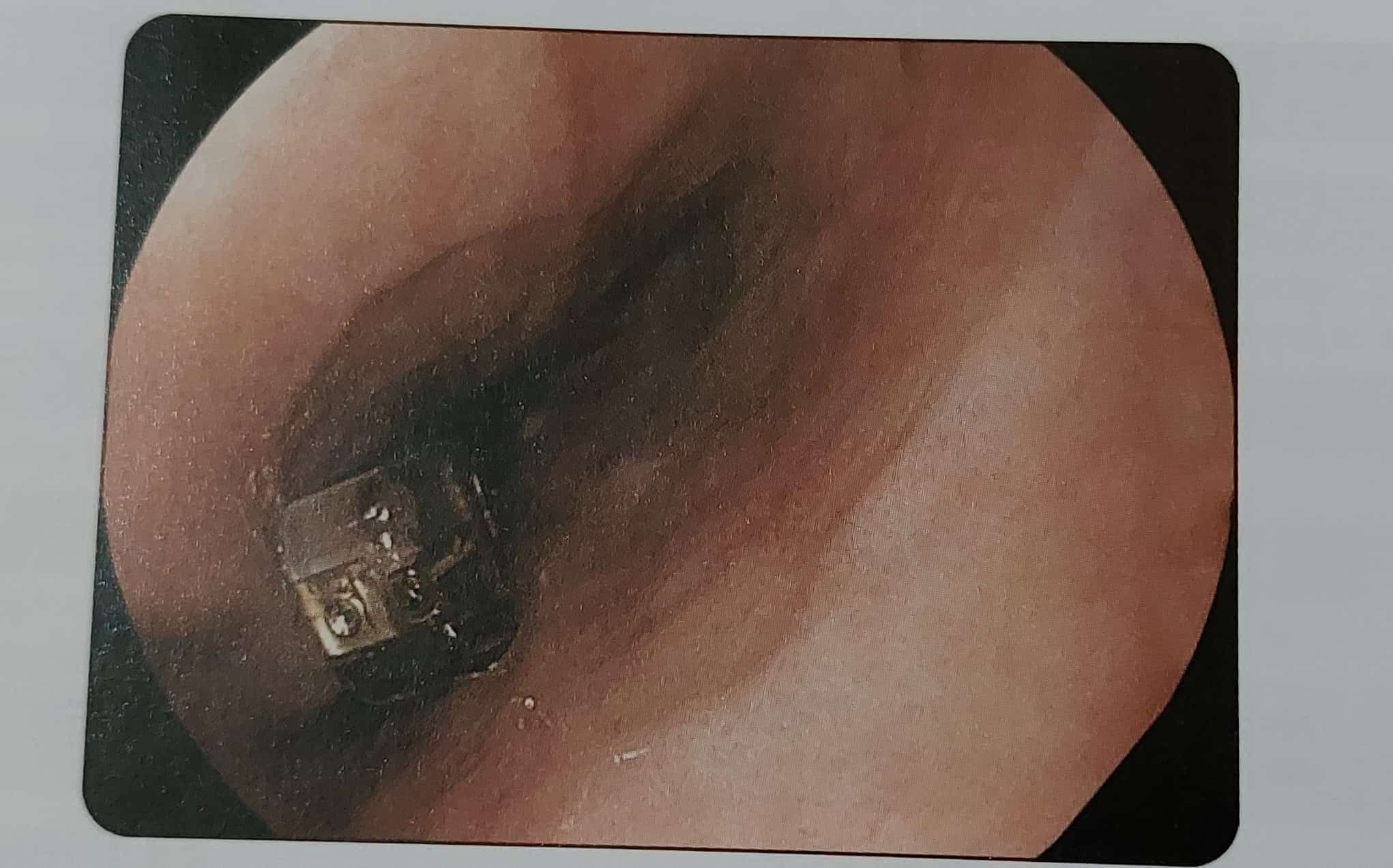
Measurement of esophageal acid exposure, i.e. the measure of acid refluxing into the esophagus, can be measured either using a catheter-based (preferably with impedance study) or a capsule-based system. In the catheter-based system, the pH electrode is placed 5 cm above the upper limit of the lower esophageal sphincter (LES) which is determined by esophageal manometry. This measurement of pH is conducted for a 24-hour period without any dietary restrictions. In the wireless capsule-based system, the pH capsule is deployed endoscopically 6 cm proximal to a squamocolumnar junction (SCI) (Fig. 2). This measurement is conducted for 48 to 96 hours, preferably off PPI therapy. This can help determine whether there is a weak or a strong correlation of patient symptoms to esophageal acid exposure. In a recent study of a large cohort of patients (n = 257) subjected to wireless pH monitoring for 48 hours versus 96 hours of testing, it was noted that prolonged wireless pH monitoring (96 vs 48 hours) increased the diagnostic yield of abnormal acid reflux by 17.5%.
| Gastrointestinal cancer in first-degree relatives |
| New onset dyspepsia in patient ≥60 years |
| Evidence of gastrointestinal bleeding (hematemesis, melena, hematochezia, occult blood in stool |
| Iron deficiency anemia |
| Anorexia |
| Unexplained weight loss |
| Dysphagia |
| Odynophagia |
| Persistent vomiting |
| Gastrointestinal cancer in a first-degree relatives |
| Duration of GERD of at least 5-10 years |
| Age 50 years |
| Male gender |
| White race |
| Hiatal hernia |
| obesity |
| Nocturnal reflux |
| Tobacco use (past or current) |
| First-degree relative with Barretts esophagus or esophageal adenocarcinoma |
IMPEDANCE TESTING
This is a catheter-based test that detects bolus movements within the lumen of the esophagus by measuring changes in resistance to alternating current when the food/air bolus passes a pair of metallic rings mounted on the catheter. It is typically a 24-hour test but is not required for the diagnosis of GERD. It is usually indicated in GERD patients who have continued symptoms despite PPI therapy and helps differentiate between acid and nonacid esophageal exposure. Such testing can help determine true GERD from symptoms of either esophageal hypersensitivity or functional heartburn.
ESOPHAGEAL MANOMETRY
Similar to impedance testing, this modality is not required for diagnosing GERD. However, it is required to exclude esophageal motility disorder in patients with atypical symptoms like chest pain or dysphagia or as a part of a preoperative workup prior to antireflux surgery. It can also be utilized to determine the location of the LES for pH testing as mentioned above. A recent study published in the Indian Journal of Gastroenterology evaluated the role of esophageal manometry and 24-hour pH testing in patients with refractory reflux symptoms. Using esophageal motility and pH testing, it was concluded that 68.3% of patients had a definitive diagnosis of GERD whereas 31.7% had non-GERD conditions such as motility disorders, functional heartburn, or hypersensitive esophagus.”
Also read: Gastroesophageal reflux disease
CONCLUSION
The overall approach to diagnosing GERD is quite straightforward when patients have typical symptoms such as heartburn and/or regurgitation but can be challenging if symptoms are atypical or related to esophageal hypersensitivity or functional heartburn are causing symptoms. A simple algorithm (Flowchart 1) can be utilized toward making an appropriate diagnosis of patients with GERD symptoms.
