Table of Contents
Gastroesophageal reflux disease
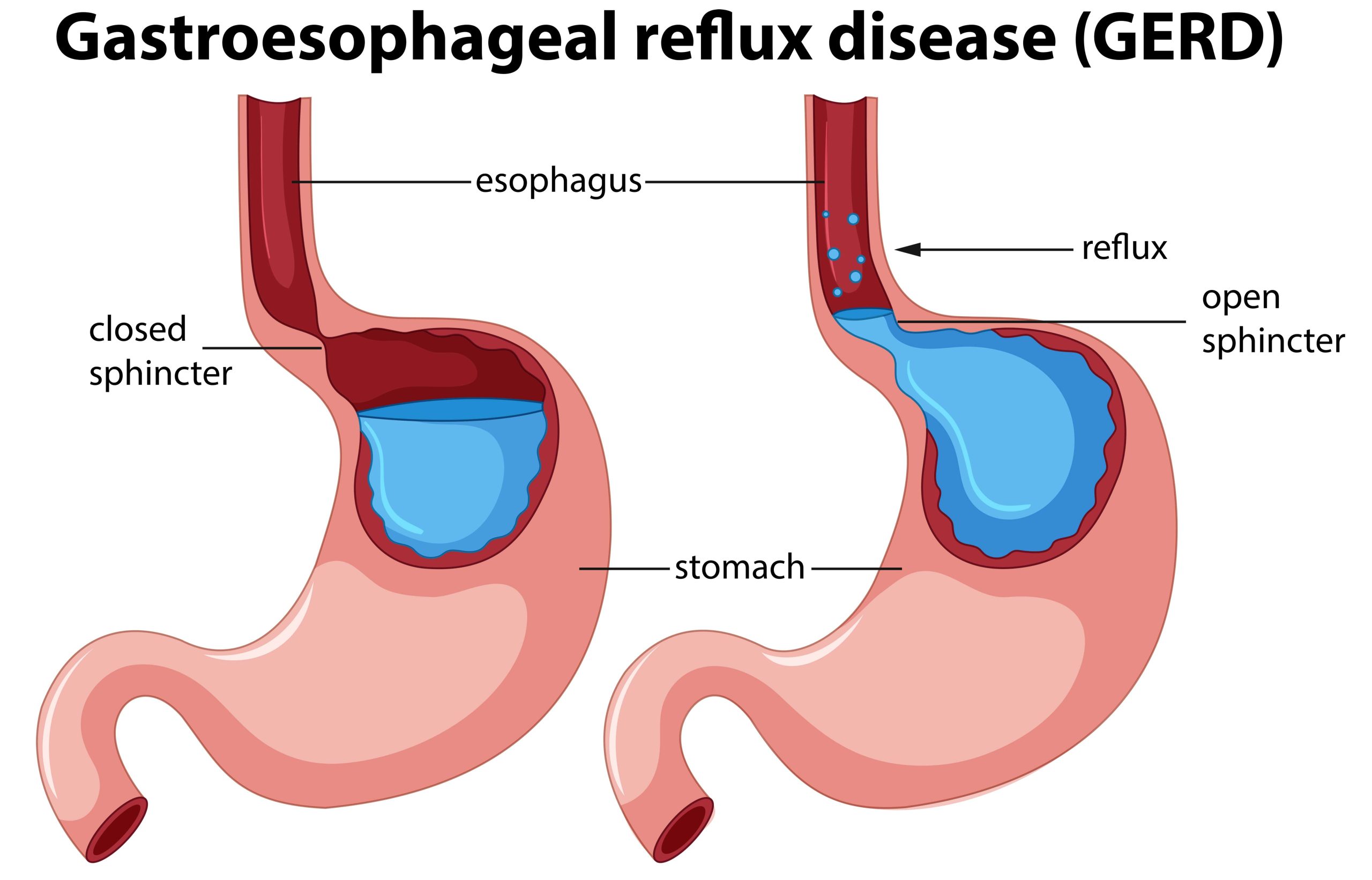
As per the Montreal definition, gastroesophageal reflux disease (GERD) is defined as a condition that develops when gastric contents reflux into the esophagus, and cause bothersome symptoms and/or complications. Physiologically, occasional reflux is common, it is considered a disease if it causes symptoms and complications.
Symptoms of GERD are classified as esophageal syndrome and extraesophageal syndromes. The esophageal syndromes are further classified into symptomatic or syndromes with esophageal injury. (esophagitis). Reflux-induced cough, laryngitis, asthma, and dental erosion are extraesophageal symptoms with established association with GERD,
The most frequent symptoms of GERD are heartburn and sour regurgitation. Heartburn is a burning sensation in the retrosternal area, and sour regurgitation is the awareness of the flow of gastric content into the mouth or pharynx. The clinical diagnosis of GERD can be made when the patient has heartburn alone or in combination with sour regurgitation, with high specificity (89-95%), but with very low sensitivity (6-38%). Approximately 30-50% of patients with GERD have symptoms of dyspepsia and/or irritable bowel syndrome. Heartburn, regurgitation, and noncardiac chest pain are GERD symptoms that originate from reflux-related sensory stimulation of the esophageal mucosa, whereas belching may be due to aerophagia resulting in supra gastric belching. The extra-esophageal symptoms of GERD include chronic cough, asthma, chronic laryngitis, and Globus sensation. Most patients with these symptoms also have classical symptoms of GERD.
Almost one-third of asthmatic patients have GERD. GERD may worsen during an episode of airway obstruction, and may also trigger an asthmatic attack by causing bronchospasm. Chronic cough is associated with reflux symptoms in more than 30% of patients. Noncardiac chest pain (NCCP) may occur due to GERD, esophageal motility disorders, and visceral or central hypersensitivity. GERD is seen in 25-60% of patients with NCCP; some patients also have erosive esophagitis.
Nocturnal symptoms in GERD are common and associated with sleep disturbance. Most patients with nocturnal symptoms have volume reflux, and hence develop regurgitation in the lying down position. Some of them also have delayed gastric emptying and ineffective esophageal peristalsis, This adversely affects their quality of life.
Symptom prevalence
In 2005, a systematic review of studies estimated that the prevalence of GERD, defined as heartburn and/or regurgitation occurring on at least 1 day per week, was 10-20% in Western countries, and approximately 5% in Asia. Currently, the global prevalence of GERD, based on the frequency of weekly heartburn is estimated to be around 13%. These figures are likely to underestimate its true prevalence since many patients self-medicate and/or do not seek medical advice; in addition, the methods to assess symptoms are variable between studies. The overall prevalence of GERD in Asia is reported to be lower than that of the developed nations, but there are regional variations, and India is among the nations with a higher prevalence.
Indian data: Data from both community and hospital-based studies suggest that (Gastroesophageal reflux disease) GERD is common in India irrespective of geographical or rural/urban location. Among the community-based studies, the largest one was from Tamil Nadu, and included 6174 subjects; the prevalence of GERD symptoms was 8.2%. The prevalence was lower in rural areas (5.07% vs 11.1% in the urban area). In a community-based study from Kerala, where the GerdQ questionnaire was used, the prevalence of GERD symptoms was higher than in other Indian studies (22.2% of 1072 individuals). The prevalence in urban areas was higher (29% vs 19%). The population-based study from Ladakh found that the prevalence in urban areas was lower (13% vs 23%) as compared to rural areas. The overall prevalence was 18.7%. A recent community-based study from central India found that 10.7% of 2774 subjects in rural settings had GER symptoms (defined as heartburn at least twice/week).
The Indian Society of Gastroenterology (ISG) task force on GERD conducted a study where data were collected from multiple states across the country. The prevalence of GERD was 7.6% among the 3224 participants. (southern India 8.35% vs northern India 6.74 %). Thus, the prevalence of GERD from hospital-based studies has ranged from 15 to 30%, and from community studies around 10% (except for one study from Kerala). Overall, these data suggest that GERD is a common problem in India with the disease burden higher than the rest of Asian countries. The symptoms of GER are more frequent in individuals >50 years of age, women, and individuals with lower levels of education and lower socioeconomic status. Individuals living in urban areas also have a higher risk of GERD.
Product to manage your acidity:
Risk factors
Based on a genome-wide association meta-analysis of 71,522 GERD cases and 261,079 controls of European descent causal roles of obesity, diabetes, and smoking have been implicated in the development of GERD. The environmental risk factors for GERD include obesity, smoking, an increase in intra-abdominal pressure, and certain dietary factors,
Multiple dietary and lifestyle factors have been implicated as risk factors for GERD. Obesity causes increased intra-abdominal pressure and is associated with hiatal hernia and altered the function of the gastroesophageal junction. Multiple studies have shown that obese patients are 1.5 to 2 times more likely to have GERD as compared to nonobese individuals. Community-based studies from India have also shown a higher risk of GERD with BMI >25 kg/m².
In support of obesity being a risk factor for GERD, there is a decline in reflux symptoms that is proportional to the degree of weight loss and reduction in BMI. Reducing the BMI by at least 3.5 kg/m² increases the odds for the disappearance of GERD symptoms by 1.5- to 2.4-fold.
Smoking and consumption of tobacco have been linked with GERD. The results from the meta-analysis of global studies as well as Indian data show an increased risk of GER symptoms with smoking. Recent data from India suggest that ingestion of carbonated soft drinks is associated with reflux symptoms.
Dietary factors are often considered as a trigger for reflux symptoms but data supporting this is weak. As there are many items in the diet, studying the effect of individual factors is challenging. Diets low in fruits and fiber, and highin sweets, spices, and fat are associated with GERD symptoms. Some studies from India show that meat consumption and decreased milk intake were associated with GERD symptoms. However, patients often report symptom aggravation after ingesting sweets, fried foods, spices and beverages. Though many patients complain of symptoms triggered by tea and coffee, a meta-analysis showed no association of (Gastroesophageal reflux disease) GERD with coffee intake.
Helicobacter pylori infection occurs in the gastric mucosa and is a causative factor for peptic ulcer as well as atrophic gastritis; multiple studies have investigated the association of H. pylori and GERD. The prevalence of reflux esophagitis is less common in patients with H. pylori infection as compared to those who are not infected. After H. pylori eradication therapy, these patients develop de novo symptoms of GERD. Thus, H. pylori infection appears to have a negative association with GERD, especially in Asian patients.
Also, read: Define emulsion, describe the preparation of an emulsion
Prevalence of esophagitis and complications of GERD
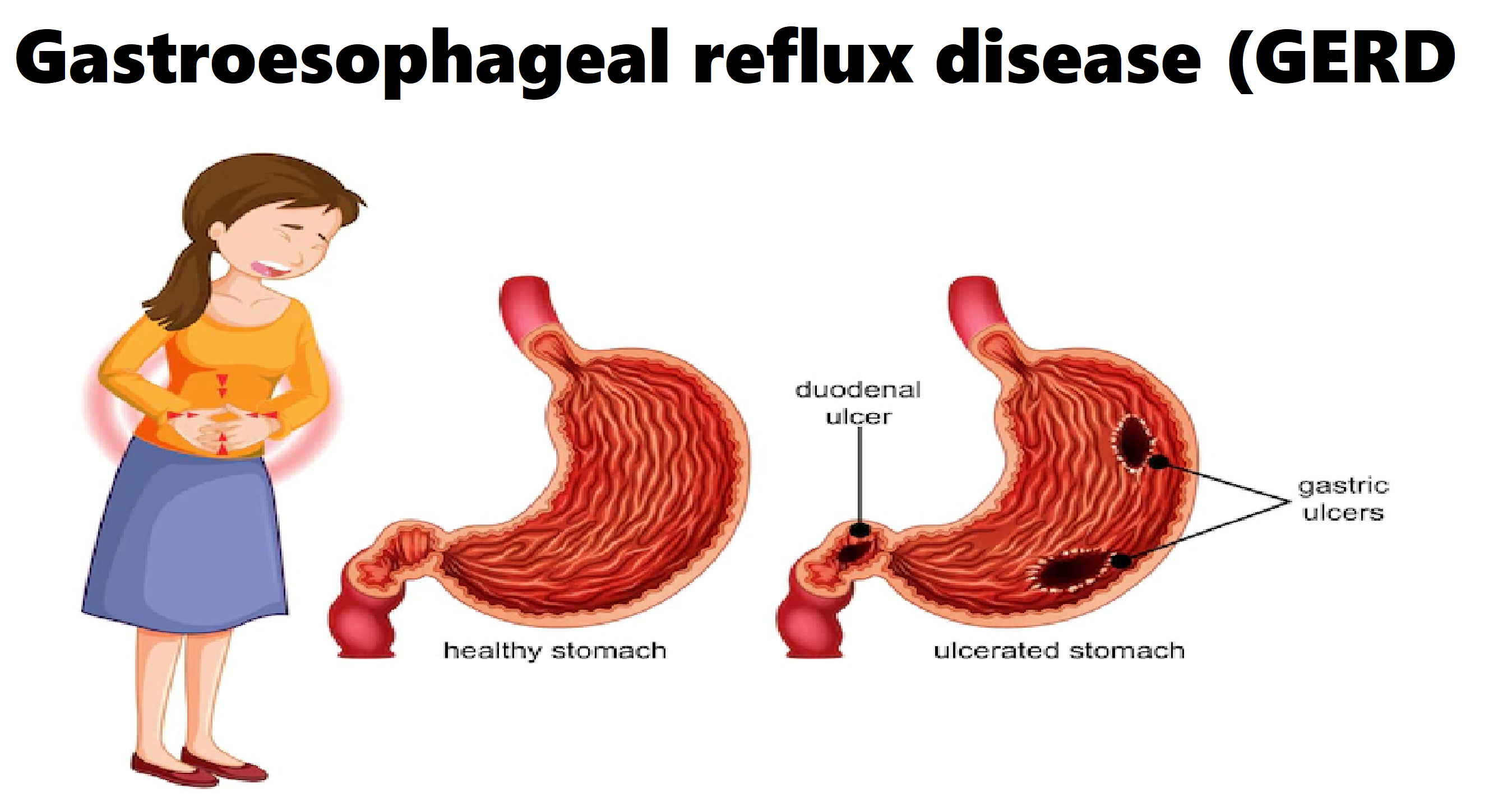
Mucosal damage due to reflux is manifested as esophagitis which is present in the distal third of the esophagus. Esophagitis is graded at endoscopy using the Los Angeles grading system, where Grade A is the mildest injury and Grade D is the severe injury. Most endoscopy-based studies have been conducted in tertiary care hospitals on subjects with upper gastrointestinal symptoms. Therefore, the true prevalence of esophagitis in the community cannot be assessed. A majority of patients with reflux symptoms have a normal endoscopy (non-erosive reflux disease [NERD]). In most studies, less than 20% of symptomatic patients have erosive esophagitis at endoscopy; in fact, esophagitis was found in <10% of Indian patients in one study.
Though the frequency of reflux symptoms in men is almost similar or less than in women, the frequency of erosive esophagitis and complications like Barrett’s esophagus and esophageal adenocarcinoma is much higher in men than in women. Barrett’s esophagus and esophageal adenocarcinoma have been found to be inversely associated with H. pylori infection. Complications of reflux like Barrett’s esophagus are associated with white race, older age, and male gender, long duration of reflux symptoms, abdominal obesity, and smoking.
Conclusion:
In conclusion, GERD is common in the general population; approximately 10% of normal people in India have weekly heartburn. The risk factors for GERD are obesity and tobacco use, along with a high-fat diet and spicy food. Endoscopy is often normal in most patients with GER symptoms.